After nearly 20 years of research, doctors have successfully implanted a new artificial heart model into a human patient — moving one step closer to replacing heart transplants entirely. That operation took place earlier this month here in Houston, the result of over $50 million in private and grant funding.
The Texas Heart Institute at Baylor St. Luke's Medical Center and California-based medical device company Bivacor completed the successful implantation of a total artificial heart, or TAH, into a human patient on July 9. The surgery was performed as part of an early feasibility study authorized by the Food and Drug Administration. Dr. William Cohn, a surgeon at the Texas Heart Institute and Baylor College of Medicine and chief medical officer at Bivacor, described the operating experience as “surreal.”
“You remember taking an exam in college, where you walk in wondering if you prepared enough? We did everything we possibly could in anticipation of this case,” Cohn said in an exclusive interview with the Houston Business Journal. “The number of acute and chronic animal cadavers, training with the surgeons, each surgeon would come here, I’d take them down here and show them how to put [the device] in an animal, and then they would do it several times with me proctoring.”
Artificial heart technology isn’t new, especially at Baylor, where the first successful heart transplant in the United States was performed by Dr. Denton A. Cooley in 1968.
But Bivacor’s TAH can sustain life for patients with a broader range of conditions than existing pumps. And while Cohn and Dr. Joseph Rogers stopped short of calling the device a complete replacement for heart transplants, they noted that this TAH is the strongest candidate yet for one of modern medicine’s holy grails — a completely synthetic heart.

“The great analogy I heard was that the hope that heart transplantation would be the solution for heart failure is akin to hoping that winning a lottery would cure poverty,” said Rogers, who is the chief executive of the Heart Institute. “There’s just not enough hearts to transplant into all the people who would need them, which has always been the driver for trying to come up with a mechanical solution that can be manufactured.”
According to the American Heart Association, heart disease has been the leading cause of death in the United States for over 100 years.
Rogers and Cohn said the first recipient of the TAH, whom they declined to identify, citing patient confidentiality rules, has been doing well since implantation. The patient is at least 18 years old, the minimum age for which the study is recruiting.
Cohn said the patient’s cardiac output, or the volume of blood being pumped by a single ventricle of the heart, was 12 liters per minute while briskly walking — a first for any patient with an artificial heart in the world. For comparison, the average natural human heart produces 5-6 liters per minute at rest, while the SynCardia Total Artificial Heart, the first TAH system to receive FDA approval, produced 10.5 liters per minute at maximum, according to a letter the company submitted to the Center for Medicare and Medicaid Services.
The HBJ reached out to Baylor College of Medicine for a cost figure for the operation but did not receive a response prior to publication.
The feasibility study is expected to run until 2026, and the first phase will enroll five patients with an FDA-mandated pause after three patients have been enrolled. According to the trial’s listing on the National Library of Medicine page, the study is recruiting in three locations in addition to Houston: Durham, North Carolina; Phoenix; and Cincinnati.
Bivacor was founded in 2008 and has a Houston seed at its heart. The company's co-founders, including the technology's brainchild and Bivacor chief technology officer Daniel Timms, were brought to the Bayou City through a $2.5 million gift from Jim "Mattress Mack" McIngvale.
"There have been so many people in Houston, Texas, who have subsequently put their resources either personally or from foundations into the development program," Rogers said. "I think this is a story that Houston should be very proud of — It's an amazing community that has gotten behind a wild, audacious idea."
Breaking barriers to heart design
Cohn said three factors that have traditionally challenged the design of artificial hearts are size, durability and the ability to pump blood without destroying it. Rogers added that most pumps are built to assist an existing heart’s left ventricle — but that leaves out patients who are suffering from failure in multiple ventricles.
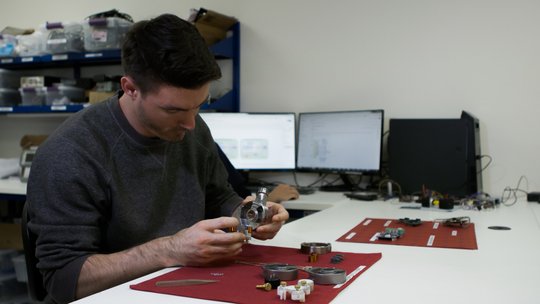
Timms proposed magnetic levitation or maglev technology to resolve all three factors of the design. He had researched the technology as part of his Ph.D. thesis in Australia. High-powered neodymium electromagnets spin a rotor that replicates the pumping function of the heart. Timms said he was surprised that unlike other artificial heart alternatives, the rotor does not significantly damage blood cells passing through the artificial heart.
"The only solution seemed to be contactless, rotating spinning discs to propel the blood [through the heart]," Timms told the HBJ. "Maglev achieves that goal with no mechanical wear — since no parts are touching anything."
The result is an apparatus roughly the size of a baseball with one moving part — the rotor. The TAH is encased in a bag made of synthetic polymers to make it easier for surgeons to operate.
An interesting aspect of the rotor motion is that the TAH does not generate a heartbeat like a natural heart, and Frazier is convinced one isn't needed for the patient to function normally. However, by regulating the speed of the rotor, a pulse can be simulated, Timms said. That pulse could be helpful for emergency responders who are checking the condition of collapsed patients with an artificial heart.
One hurdle the team is still navigating is the power source. Currently, patients in the feasibility study are remaining at Baylor under observation, and the heart’s existing battery is wired to a battery that is carried externally in a bag, along with a computer that can be monitored by physicians.
But Cohn said advances in batteries and materials science taking place at Houston institutions such as Rice University could lead to a TAH that looks not unlike Iron Man’s arc reactor.
“Every day I pick up the science section hoping you’ll describe the new arc reactor,” Cohn said. “In the ultimate configuration [of the TAH], there is no drive line, there is no wire leaving the body, but you're still going to have to have six or seven watts per hour. And so the batteries are always going to be outside the body, and we'll use inductive coupling, like the thing that charges your cell phone."
Timms said he also was looking forward to advances in miniaturizing magnets while retaining the power and magnetic field necessary to make the rotor spin efficiently.
"It's challenging to get it smaller and smaller using maglev technology. There's leakage from the magnetic fields [that affects the rotor's efficiency] that needs to be controlled as the device gets smaller," Timms said. "It's small enough to fit in a 12-year-old patient, but we could make it fit in a 5-year-old patient."
Future funding and new leadership at Bivacor
To date, Bivacor has raised $53 million in venture and grant funding, according to Crunchbase. Cohn told the HBJ the company would look at raising a Series C round sometime in the fall to stay funded during the remainder of the trial. Bivacor's most recent venture funding round was announced in 2021, though the company has secured several grants and bridge rounds since then.
Bivacor also brought in new leadership prior to the beginning of the human trial. The company hired Jim Dillon as its new CEO in January 2024 and Raymond Cohen as chair of the board in December 2023. Both men have experience leading clinical-stage companies and knew each other through one of Bivacor’s investors, Cohn said.
“We had a race car, we needed a race car driver,” Cohn said. “There are opportunities to do a public offering; there are opportunities to continue to raise venture — we've had tons of great support from the National Institutes of Health, millions of dollars in grants. There's a lot of avenues in, and we're open to all of them. But we never want that to interfere with what we're trying to do: creating something the world needs. As long as the money understands what motivates us, and is OK with that, then we're opportunistic.”
Leaders in Houston's life sciences community have said that one of the missing ingredients for the city to boost its life sciences ecosystem output is experienced management that can lead and raise funding for clinical-stage companies undergoing FDA trials, especially when companies are unable to generate revenue prior to regulatory approval.
"It's been a phenomenal amount of people that have made this happen, often at times without any funding," Timms said. "The passion of people that introduced themselves to this project because it's something the world needs, but it's also so hard to get funding — over 20 years of work is testament to that."
Sign up here for the Houston Business Journal’s free morning and afternoon daily newsletters to receive the latest business news impacting greater Houston.
The headline on this story has been corrected. Baylor College of Medicine surgeons conducted the operation for the heart, but the lead organization is the Texas Heart Institute, which is no longer affiliated with BCM.