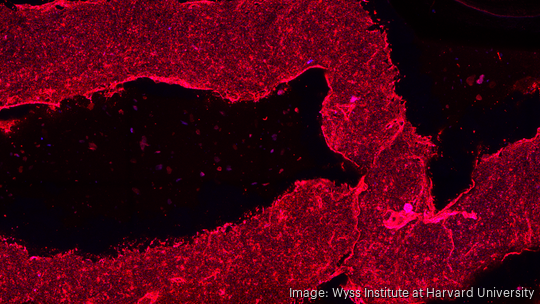
In a Harvard lab sits a two-ton block of granite. On top of that granite, a precision-motion system can successfully print multilayer vasculature — blood vessels, essentially — into various materials, including cardiac, kidney and liver tissues.
The granite is to prevent vibrations from the environment. The vessels printed by the lab are about a millimeter-and-a-half thick, and are made up in two parts, an outer shell and an inner tube. The lab can print vessels as small as 120 microns — the width of human hair
This is all being done by a team of scientists from the Harvard John A. Paulson School of Engineering and Applied Sciences (SEAS) and Wyss Institute for Biologically Inspired Engineering.
The lab — run by Jennifer Lewis, a Hansjorg Wyss Professor of Biologically Inspired Engineering at SEAS — developed what it calls "sacrificial writing in functional tissue (SWIFT)" in 2019. That method enabled them to create patterns of hollow channels in thick living tissue, which led them to create patterns of vasculature in tissue for the first time.
However, they still had to make the walls of the vessels.
The lab uses a new method, called coaxial-SWIFT (co-SWIFT), in which two needles, one inside the other, extrude two different materials simultaneously. The needles, known as the coaxial bioprinting nozzle, enable the lab to create a vessel wall inside and the shell of a blood vessel around it.
“It's just two needles, one inside of the other. One part extrudes the shell — the wall of the vessel — and the other part extrudes the gelatin, which, when we heat it up, melts away, leaving behind a hollow channel,” said Paul Stankey, a fourth bioengineering Ph.D. student at SEAS in the lab of co-senior author Jennifer Lewis.
- Sign up for The Beat, BostInno’s free daily innovation newsletter. See past examples here.
What’s special about the co-SWIFT method is that it allows Stankey and the lab to create interconnecting systems of blood vessels. What’s hard about the co-Swift method is that everything is really small. The connections being made to create the vascular systems are no wider than a single human hair.
Stankey and the lab also have to ensure that the material is rigid enough to stay in place, but loose enough to move if need be is difficult. When Stankey is trying connect two vessels there’s even less margin for error because the whole system can break if the connection is missed.
The development allows the lab to move forward in two significant ways, according to Stankey. The first is that it allows the lab to build “massive tissues” via 3D printing. The second is that the lab can begin thinking about moving these tissues into animals and eventually into people.
With the new co-SWIFT method, the lab can even manufacture patient-specific structures. Stankey was able to print the left coronary artery and its main branches by taking a CT scan of a patient.
“The best way to think about it is like you're building a house. So at the same time that you're putting up all the scaffolding, which you should think of as the main cell types think of the blood vessels as the electrical wiring,” said Stankey. “So you need to build these at the same time. And so they all come together in the end to finish the house, to finish the organ that you're trying to manufacture.”








