The pandemic fueled changes in health care delivery in a way that we’ve never seen before. People were at home, especially during the shutdowns, but at the same time people still needed care and physicians needed to operate their businesses.
This created a unique moment for embracing innovation. We had groups that may have been more averse to technology in the past going all in on different kinds of solutions. Whether it was the doctor who still keeps paper records or the member who is still learning how to use a smartphone. All of a sudden, the COVID-19 crisis forced these types of people out of their comfort zones and we saw them coming together to use technology in totally new ways.
These changes range from micro to macro-level – they started with physicians and patients meeting over the phone, video chats, and it was ad hoc for the most part, but over the course of the last year and a half, the infrastructure has become much more robust, and an openness to innovation is more formally cemented into our health care delivery system.
We’re in a world where people expect goods and services when they want them and how they want them. For the most part, other industries have been driving this. However, in this environment, people expect the health care system to move as quickly and efficiently as any of the other industries with which they do business – and before the pandemic, the health care system just was not keeping up.
In this article, I will outline how innovation is starting with consumer demand, expanding to ways of working between payers such as health insurers and providers such as hospitals, and ultimately, leading to opportunities for sweeping changes that will transform the system overall.
Offering new options for consumers
Before the pandemic, virtual care was something that industry leaders were hoping would take off. There was investment happening in the space, bets being made, but the demand was low. The shift that happened during the pandemic was in consumer demand – people started to access care differently, and because of the work that had been happening all along in this space, we were ready to meet consumers with new tools.
For example, we offer our members access to virtual visits through LiveHealthOnline. Before COVID, we saw people using this kind of technology for an urgent health need – think of it as a quick opinion needed to help get someone to the next step…e.g., do I need to go to the emergency room or can I wait until tomorrow? But now, we’re seeing usage grow in specialty areas like allergy, dermatology, and maternity care. It’s going beyond that quick assessment and become much more ubiquitous. As part of our mission to materially and measurably improve the health of New Yorkers, we’re excited to have new options for delivering care that people need, when they need it, in a way that works for them.

Building on this, one innovation that we’re working on with our parent company is called Anthem Link, and it went live in January 2021 on our Connection network in New York (only available in small group segment, which includes, for example, small businesses with under 100 employees). Anthem Link is an innovative, integrated product that is driven by our latest technology and digital solutions. It seamlessly connects our high-quality, high-performance networks with digital innovations.
The digital aspect of it is differentiating, and what we’re really excited about. We’re bringing savings, with new ways to access health care. Leveraging our award-winning mobile app, Sydney Health, Anthem Link members will have access to features to help direct them to the most cost-effective care in the most appropriate setting as well as tools to help them manage their health and wellness. Featured tools include: convenient care via text-based chat or secure two-way video; AI-powered symptom checker helps direct consumers to the most appropriate treatment; custom curated member digital content; digital action plans, tracking and rewards; digital lifestyle coaching (and virtual telephonic) and digital maternity support via LiveHealthOnline Lactation.
It’s an example of our strategy to build next-generation managed care solutions driven by a combination of digital engagement, integrated guidance, networks, and benefit design.
Enhancing data integration between health insurers and providers to power value
With the tremendous shift to digital since the start of the pandemic, we have such an opportunity to improve our health care system, and drive affordability using data. We are encountering a moment, unlike any before, where the environment is ready for new ways of engaging. However, the current flow of information between providers such as hospitals and health insurers relates to just claims and billing and doesn’t take full advantage of the technology available to us.
Additionally, any flow of data between health care providers and health insurance plans is often in one direction and slow – leading to ineffective collaboration. This lack of communication and coordination can frustrate providers and consumers, and – more importantly – potentially delay care or lead to poorer health outcomes.
Real-time, bi-directional exchange of data between stakeholders such as health insurance plans and hospitals will help us take the next step in health care’s digital evolution. In 2020, Empire set a goal to have 80% of our members connected to us with real-time admissions, discharge and transfer notifications from providers such as hospitals and access to electronic medical records (ADT/EMR) data by the end of 2022. Over the longer term, we are also working to give providers data-driven, insights from our Empire members – across different EMR systems – as well as automate some aspects of providers’ workflow to improve – or even automate – processes like prior authorization for health care procedures.
Building a platform as a lifetime, trusted health partner
Achieving whole-person health requires taking a more holistic view of health and leveraging data that allows us to see and address the most impactful drivers of health. When stakeholders have ready, secure access to both individual consumer information and population-level health data, the health care system will work better for consumers and their care providers by reducing administrative delays, lowering costs, and delivering more actionable insights.
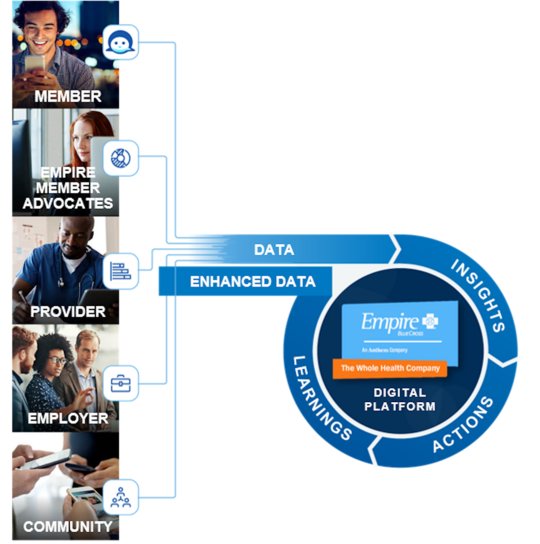
Anthem, Inc., Empire’s parent company, is becoming a platform for health to transform from a health insurance company to a lifetime, trusted health partner. We are building a health care system that works better for everyone – simpler, more affordable, and more accessible. Part of this effort is through our Health OS platform – a comprehensive, cloud native, payer and provider agnostic platform. It leverages a vast amount of data and offers predictive analytics; AI-driven tools; machine-learning; reduction in administrative burden; and real-time, more stable insights to produce proactive, personalized solutions that answer the needs of our consumers, health care providers, employers, and communities.
The health care system needs these types of upgrades to create a new kind of healthcare ecosystem – one that is powered in service of all New Yorkers – and these examples from big to small demonstrate how we can use innovation to significantly improve the way we work.
Serving the 11 eastern and southeastern counties of New York State, Empire BlueCross is on a mission to materially and measurably improve the health of New Yorkers. In 2020, Empire BlueCross was named one of Albany Business Review’s Best Places to Work. Additional information about Empire is available at www.empireblue.com.
Alan J. Murray is president and CEO of Empire BlueCross. He is on a mission to materially and measurably improve the health of all New Yorkers. Through his leadership and expertise, he is determined to power the health care system with game-changing innovation that benefits customers and providers across New York.